Urological Oncology
Urological oncology has undergone substantial advancements in diagnostics, surgery, and pharmaceuticals within the last five years, significantly benefitting patients with testicular, bladder, kidney, and prostate cancer under the care of A/Prof Zargar. Prostate cancer diagnosis, in particular, has witnessed improvements with the evolution of MRI machinery and other modern imaging and biopsy techniques.
In addition to diagnostic enhancements, the field has seen progress in genomics, offering tailored treatment strategies through commercial multiplex gene panel tests for kidney, bladder, and prostate cancer patients. A/Prof Zargar also collaborates with a multidisciplinary team to offer the latest pharmaceutical therapies, including immunotherapies, novel therapies, and targeted agents, based on the most recent evidence or access to clinical trials. Surgery remains a primary approach in urological cancer treatment, with A/Prof Zargar specializing in a wide range of oncological procedures, often performed minimally invasively with robotic technology.
bladder cancer
Bladder cancer, mainly transitional cell carcinoma (TCC) also called urothelial carcinoma of the bladder , constitutes about 3% of annual cancer diagnoses in Australia.
Early-stage bladder cancer may not exhibit noticeable symptoms but can lead to microscopic blood in routine urine tests.
Common symptoms include painless intermittent haematuria, a burning sensation during urination, and urinary frequency/urgency.
These symptoms, akin to urinary tract infection signs, warrant further investigation if an 'infection' persists despite antibiotics.
Risk factors encompass smoking, occupational exposure to certain chemicals, specific drugs, pelvic radiotherapy, prolonged bladder inflammation, and rare conditions like schistosomiasis.
Superficial bladder cancer, confined to the bladder lining, constitutes 75% of new diagnoses and can be initially managed with local treatments.
Muscle-invasive bladder cancer, life-threatening and extending into the bladder muscle, may require extensive assessments and treatment options, including radical cystectomy or a combination of radiotherapy and chemotherapy.
Kindey cancer
Kidneys filter blood and eliminate waste through urine, making them susceptible to cancer like any other organ. Kidney cancer constitutes approximately 3% of annual cancer diagnoses in Australia, with renal cell carcinoma (RCC) being the most common form.
RCC, originating from the kidney's microscopic tube system, often grows slowly without noticeable symptoms until reaching a considerable size.
Advances in imaging technology have led to the incidental detection of RCC during scans performed for unrelated reasons, enabling early-stage identification with a high cure rate through surgical removal.
Pre-operative diagnosis is possible through needle biopsy, but due to the high likelihood of malignancy, surgery often precedes a definitive diagnosis.
Treatment Approaches:
Observation: Small, slow-growing tumours (<4cm) may be monitored with regular scans, especially in the presence of other health concerns.
Surgery: The gold standard for treatment, involving radical nephrectomy for larger tumours and partial nephrectomy for smaller ones.
Ablation: Depending on tumour size and location, alternatives like radiofrequency ablation or high-dose radiotherapy may be considered to avoid surgery.
Treatment choice depends on tumour type, clinical circumstances, and patient preferences, emphasizing individualized care.
Ongoing studies explore innovative approaches like different forms of ablation, showcasing the evolving landscape of kidney cancer treatment options.
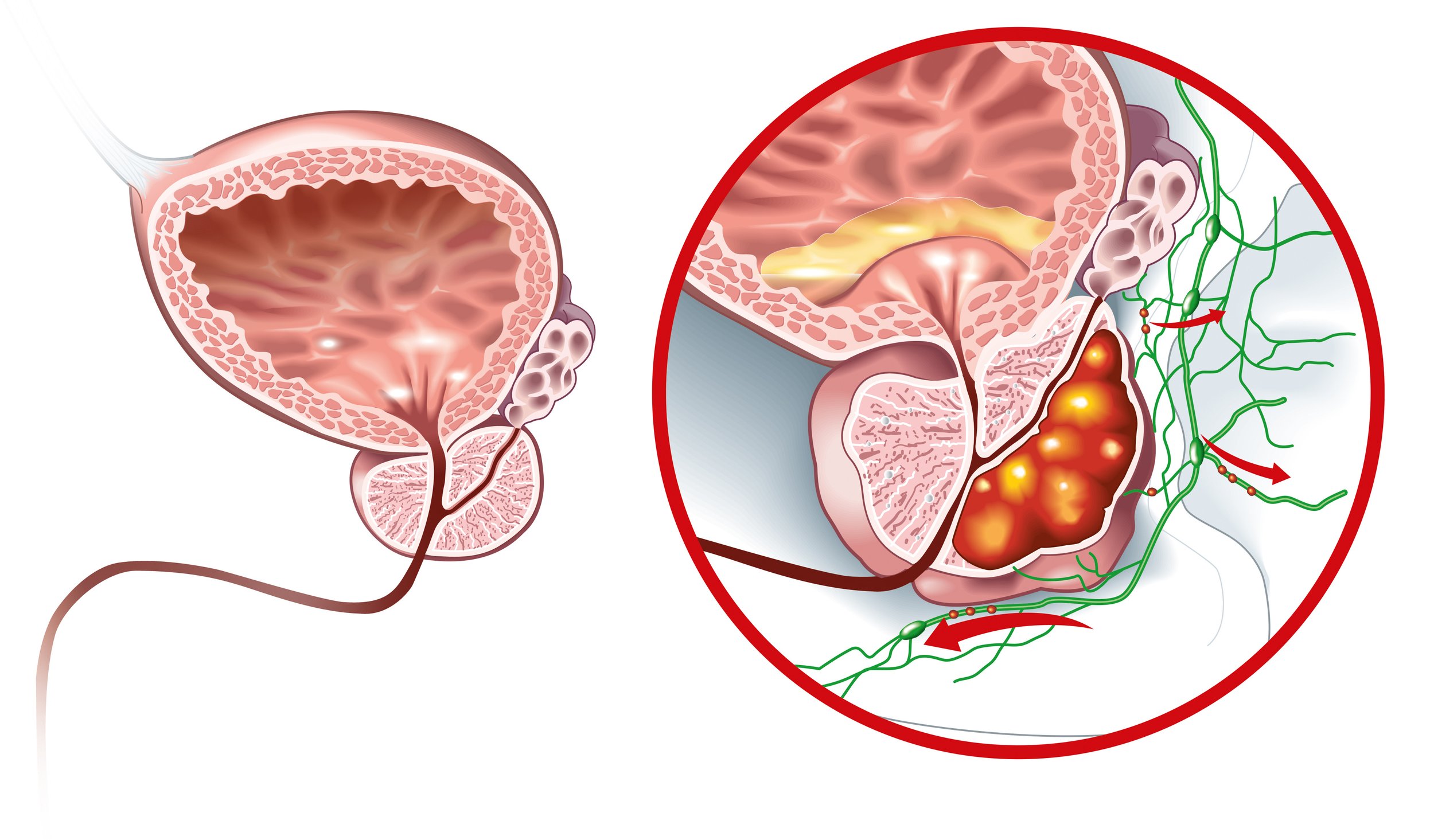
prostate cancer
Prostate cancer predominantly targets the outer part of the gland, typically exhibiting slow growth over several years. Approximately one in six Australian men is diagnosed with prostate cancer during their lifetime.
Often asymptomatic until locally advanced or spreading to other body parts.
Prostate cancer stands as the second most prevalent cause of cancer-related death in men.
Risk factors encompass family history, age, genetics, and dietary factors.
Prostate Specific Antigen (PSA) in the blood, elevated when prostate cells become cancerous, is a screening test; however, only around one-third of men with elevated PSA are diagnosed with prostate cancer.
Symptoms, when present, include urinary issues associated with benign prostatic hyperplasia (BPH).
Advanced stages may cause pain, especially if the cancer spreads to bones.
Diagnosis involves assessing risk factors, a digital rectal examination (DRE), and a prostate biopsy.
Early detection is crucial, and a prostate biopsy confirms cancer presence.
Prostate cancer necessitates vigilant monitoring and tailored treatment based on the disease's characteristics and individual circumstances.